Low sexual desire affects millions of women, but conversations about treatment remain frustratingly rare. In this evidence-based guide, read about Addyi (flibanserin), the first and only FDA-approved medication specifically designed to treat hypoactive sexual desire disorder in women.
Low sexual desire affects millions of women, but conversations about treatment remain frustratingly rare. In this evidence-based guide, read about Addyi (flibanserin), the first and only FDA-approved medication specifically designed to treat hypoactive sexual desire disorder in women.
If you've noticed your interest in sex has significantly declined and it's bothering you, you're not alone. Approximately one in ten women experiences hypoactive sexual desire disorder (HSDD), making it one of the most common female sexual concerns. Yet many women suffer in silence, unsure whether their experience is normal or if help is available.
Let's talk honestly about Addyi (flibanserin), the first FDA-approved medication for treating low sexual desire in women.
Why This Matters Now More Than Ever
For decades, women's sexual health has been dismissed, minimized, or simply not talked about. When Viagra was approved in 1998 for men's erectile dysfunction, it took just six months. When Addyi was submitted for approval to treat women's low desire, it took six years and required clinical trials three times larger than those for Viagra.
This isn't just about medication. It's about recognizing that women's sexual wellbeing matters.
Here's why this conversation is so important:
Sexual desire affects quality of life. For many women, loss of desire creates feelings of disconnection, inadequacy, and frustration. It can strain even strong relationships and chip away at your sense of self. Sexual intimacy is a legitimate part of human wellbeing, not a trivial concern.
Women's health is finally getting the attention it deserves. We're living in a time when women are increasingly refusing to accept that their health concerns are "just part of being a woman" or "all in your head." From endometriosis to menopause to sexual dysfunction, women are demanding, and receiving, better research, better treatments, and better conversations.
This affects more women than you might think. HSDD is more prevalent than erectile dysfunction, yet it receives a fraction of the attention and research funding. An estimated 6 million premenopausal women in the U.S. alone have HSDD, and that number increases significantly when you include postmenopausal women.
Awareness is still remarkably low. Many women, and even some healthcare providers, don't know HSDD is a recognized medical condition with treatment options. Women often blame themselves, their partners, or their busy lives, never realizing there could be a neurobiological component at play.
The stigma is real and harmful. Society sends mixed messages to women about sexuality: be desirable but not too sexual, prioritize everyone else's needs but also maintain a healthy sex life, and certainly don't complain if your desire wanes. This stigma keeps women from seeking help and doctors from asking the right questions.
Understanding that low sexual desire can be a treatable medical condition, not a personal failing or inevitable part of aging, is genuinely life-changing information for many women. Whether or not Addyi is right for you, simply knowing that your experience has a name, that it's common, and that help exists can be incredibly validating.
What Exactly is HSDD?
Hypoactive sexual desire disorder isn't just about occasionally not being in the mood, that's completely normal. HSDD is diagnosed when you experience a persistent or recurrent absence of sexual desire that causes you personal distress or creates difficulties in your relationship.
Here's what makes it a disorder rather than just a normal fluctuation:
- You used to have sexual desire, but it's significantly decreased or disappeared
- The low desire happens regardless of the situation, partner, or type of sexual activity
- It's been going on for at least six months
- It's causing you distress, you feel frustrated, sad, worried, or like you've lost part of yourself
- It's not caused by another medical condition, medication side effect, relationship problem, or mental health issue
That last point is important. If your low desire stems from untreated depression, a medication you're taking, or serious relationship problems, those underlying issues need to be addressed first.
Read: What Causes a Low Sex Drive During Perimenopause? (And How To Navigate It)
Is This Just "Female Viagra"?
No, and this is a crucial distinction. Viagra works on blood flow to help with physical arousal in the moment. Addyi works completely differently, it's a daily medication that affects neurotransmitters in your brain, specifically targeting the neural pathways involved in sexual desire.
Think of it this way: Viagra is about the body's response, while Addyi is about the brain's interest. Addyi addresses dopamine, norepinephrine, and serotonin levels to help restore the balance needed for sexual desire. It's not a hormone, and it's not something you take right before sex.
Does It Actually Work?
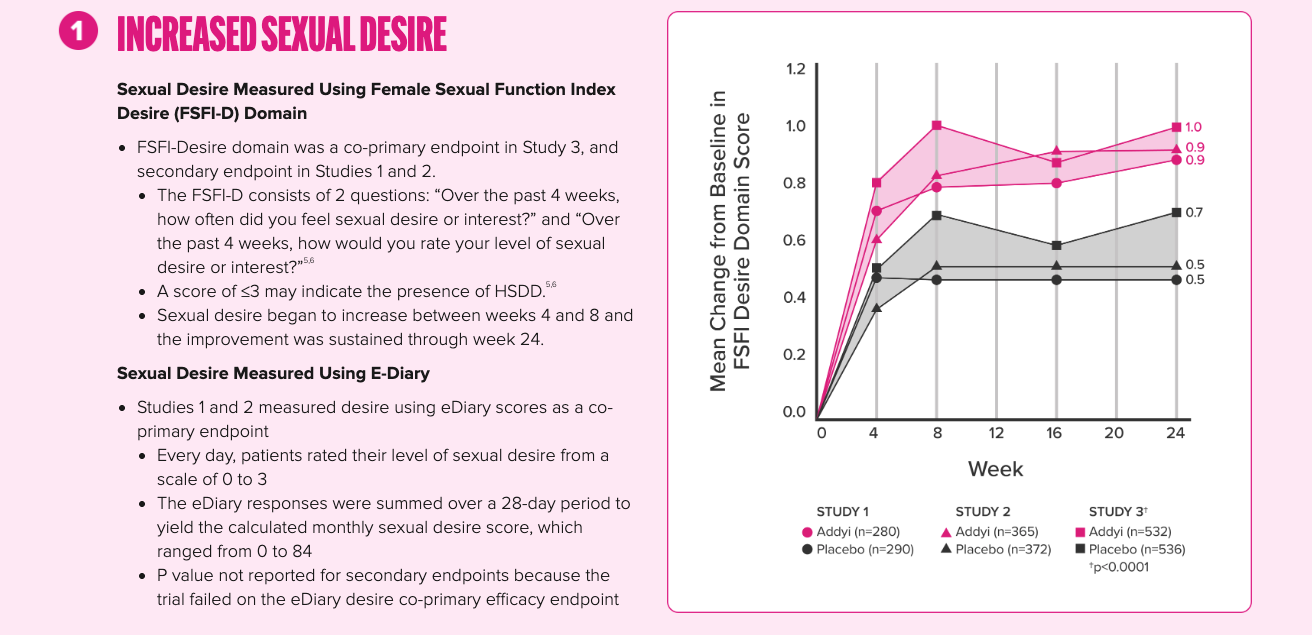
Let's be honest about what the research shows. In clinical trials involving over 2,000 women, approximately 46-60% reported meaningful improvement. That means it works for a little more than half of the women who try it, but not everyone.
Women who benefited from Addyi reported:
- Increased sexual desire
- More satisfying sexual events per month
- Decreased distress about their low desire
Improvements typically start around four weeks, though they can be subtle at first and build gradually. Some women notice changes earlier, while others need more time. If you haven't seen any benefit after several months, it may not be the right treatment for you.
What About the Alcohol Restriction?
This is probably the most talked-about aspect of Addyi, and understandably so. Here's the straightforward answer:
Combining Addyi with alcohol can cause severe low blood pressure and fainting. The rules are clear:
- If you have 1-2 standard drinks in the evening, wait at least 2 hours before taking your bedtime dose
- If you have 3 or more drinks, skip that night's dose entirely
- After taking Addyi at bedtime, don't drink alcohol until the following day
A standard drink is one 12-ounce beer, 5 ounces of wine, or 1.5 ounces of spirits.
Is this manageable? That depends on your lifestyle. If you rarely drink or can plan around the timing, it may not be an issue. If you regularly enjoy evening cocktails or wine with dinner, you'll need to adjust your habits or consider whether this medication fits your life.
What Are the Side Effects?
The most common side effects, occurring in more than 2% of women in trials, include:
- Dizziness (11.4%)
- Sleepiness (11.2%)
- Nausea (10.4%)
- Fatigue (9.2%)
- Insomnia (4.9%)
- Dry mouth (2.4%)
Most of these effects begin within the first two weeks of starting the medication and often improve over time. This is why Addyi must be taken at bedtime, taking it during waking hours increases the risk of these side effects significantly.
Some women also report anxiety, constipation, or abdominal discomfort, though these are less common.
In clinical trials, women did not typically gain weight on Addyi. In fact, there was a slight tendency toward weight loss.
Who Shouldn't Take Addyi?
Addyi isn't safe for everyone. You should not take it if you:
- Have liver problems (it's contraindicated)
- Are taking certain medications, particularly moderate or strong CYP3A4 inhibitors (like some antifungal medications)
- Drink alcohol regularly and can't modify this habit
- Are taking medications that increase flibanserin levels in your blood
You should discuss Addyi carefully with your doctor if you:
- Have low blood pressure or take blood pressure medications
- Have a history of depression or other mental health conditions
- Take other CNS depressants (medications that cause drowsiness)
- Are pregnant, planning to become pregnant, or breastfeeding
Important Update: Now Approved for More Women
In December 2024, the FDA expanded Addyi's approval to include postmenopausal women under age 65. Previously, it was only approved for premenopausal women. This is significant because many women experience changes in desire during and after menopause, and now there's an approved treatment option for this broader population.
Isn't Low Desire Just a Hormone Problem?
Not always. While hormonal changes particularly during menopause, after childbirth, or due to certain medical conditions can contribute to low desire, HSDD is often more complex. The brain's neurotransmitter balance plays a significant role in sexual desire, which is why a non-hormonal medication like Addyi can be effective.
That said, some women do benefit from hormone therapy, particularly testosterone therapy in postmenopausal women. Your doctor can help determine whether hormonal factors are contributing to your low desire and whether hormone therapy might be appropriate for you.
Understanding Your Hormone Patterns
Because hormonal fluctuations can significantly impact sexual desire, understanding your unique hormone patterns is valuable. Tools like Oova's at-home hormone tracking can help you and your healthcare provider see the full picture of what's happening with your progesterone, estrogen, and other key hormones throughout your cycle. This data can help determine whether hormonal factors are contributing to changes in your libido and guide treatment decisions, whether that's Addyi, hormone therapy, or a combination approach. Knowledge is power, and having concrete data about your body's hormone levels can lead to more targeted, effective treatment.
Are There Alternatives?
Yes. Addyi isn't the only option:
Other medications:
- Vyleesi (bremelanotide) is an injection you give yourself at least 45 minutes before sexual activity
- Testosterone therapy (off-label use in women, more established for postmenopausal women)
- Bupropion (an antidepressant that may help, especially if your low desire is related to SSRI use)
Non-medication approaches:
- Sex therapy or counseling to address psychological factors
- Couples therapy for relationship issues
- Lifestyle changes: managing stress, improving sleep, regular exercise
- Addressing underlying medical conditions or medication side effects
Many experts recommend a combined approach medication along with therapy or lifestyle modifications for the best results.
How Do I Know If I Should Try Addyi?
Ask yourself these questions:
- Did I used to have normal sexual desire that has now decreased significantly?
- Does my low desire occur regardless of the situation or partner?
- Am I distressed about my lack of sexual desire?
- Have I ruled out other causes (medications, relationship problems, untreated medical or mental health conditions)?
- Can I commit to taking a daily medication and following the alcohol restrictions?
If you answered yes to these questions, it's worth having a conversation with your healthcare provider.
Talking to Your Doctor
Many women feel uncomfortable bringing up sexual concerns, and many doctors don't routinely ask about them. But this is a legitimate medical issue, and you deserve to have your concerns addressed.
You might say something like:
- "I've noticed a significant decrease in my sexual desire over the past [timeframe], and it's causing me distress. I'd like to explore what might be causing this and discuss treatment options."
- "I think I might have HSDD. Can we talk about whether Addyi might be appropriate for me?"
Your doctor should take a complete medical history, ask about your symptoms, rule out other causes, and discuss whether you're a good candidate for Addyi or other treatments.
The Bottom Line
Addyi is a legitimate treatment option for women with HSDD, backed by clinical trials and FDA approval. It doesn't work for everyone, and it comes with important restrictions and side effects to consider. But for many women, it has made a meaningful difference in reclaiming an important part of their lives.
Low sexual desire that causes you distress is not something you need to just accept or feel ashamed about. It's a medical condition with treatment options available. Whether Addyi is right for you depends on your individual situation, but knowing the facts empowers you to have an informed conversation with your healthcare provider.
You're not broken. You're not alone. And you have options.
About the author

Sources
- "Addyi (flibanserin)." Addyi, Sprout Pharmaceuticals, 2025, addyi.com.
- "Addyi Healthcare Provider Information." Addyi HCP, Sprout Pharmaceuticals, 2025, addyihcp.com.
- Clayton, Anita H., and Sheryl A. Kingsberg. "Treatment of Hypoactive Sexual Desire Disorder Among Women." PMC, 2021, pmc.ncbi.nlm.nih.gov/articles/PMC8412154.
- "Flibanserin (Addyi)." Cleveland Clinic, 2025, my.clevelandclinic.org/health/drugs/18608-flibanserin-oral-tablets.
- "Flibanserin (oral route)." Mayo Clinic, 2025, www.mayoclinic.org/drugs-supplements/flibanserin-oral-route/description/drg-20152672.
- "Hypoactive Sexual Desire Disorder." American Sexual Health Association, 2018, www.ashasexualhealth.org/hypoactive-sexual-desire-disorder.
- "Hypoactive Sexual Desire Disorder." Sexual Medicine Society of North America, www.smsna.org/patients/conditions/hsdd.
- Kingsberg, Sheryl A., et al. "Hypoactive Sexual Desire Disorder." Mayo Clinic Proceedings, vol. 91, no. 12, 2016, www.mayoclinicproceedings.org/article/S0025-6196(16)30596-1/fulltext.
- Seehuus, Martin, and Jennifer A. Clifton. "Female Sexual Interest and Arousal Disorder." StatPearls, 2024, www.ncbi.nlm.nih.gov/books/NBK603746.
- Sprout Pharmaceuticals. "ADDYI (flibanserin) Label." U.S. Food and Drug Administration, 2015, www.accessdata.fda.gov/drugsatfda_docs/label/2015/022526lbl.pdf.
- Stein, Abigail. "A Pill for Sexual Desire Reaches a New Group of Women." TIME, 2024, time.com/7341012/sexual-desire-pill-addyi-cindy-eckert.
About the Oova Blog:
Our content is developed with a commitment to high editorial standards and reliability. We prioritize referencing reputable sources and sharing where our insights come from. The Oova Blog is intended for informational purposes only and is never a substitute for professional medical advice. Always consult a healthcare provider before making any health decisions.



